Gain In-Depth Insights into the Effects of Colitis on Your Colon Health and Overall Wellness
Colitis represents a major inflammatory disorder that significantly impacts the inner lining of the colon, which is commonly referred to as the large intestine. The inflammation caused by colitis manifests in a variety of disruptive symptoms and complications, making it a serious health concern for many individuals. The term “colitis” includes several types of inflammatory bowel diseases (IBD), notably ulcerative colitis and Crohn's disease. Each variant presents distinct challenges and features that require thorough management and thoughtful consideration for effective treatment strategies.
Understanding the intricacies of colon inflammation is crucial for appreciating its extensive effects on your overall health and well-being. When you experience intestinal inflammation, your colon may suffer from swelling and irritation, which disrupts its normal functioning and leads to a spectrum of gastrointestinal issues that can heavily impact your daily activities. Therefore, taking proactive measures to address these concerns is vital for sustaining a healthy lifestyle.
The intensity of colitis symptoms can range from mild discomfort to severe conditions that demand ongoing management. By exploring the complexities surrounding colitis, you will better navigate its many challenges and pursue appropriate medical care, ultimately enhancing your health outcomes and overall quality of life.
Critical Information You Need to Understand About Inflammatory Bowel Disease (IBD)
- Colitis signifies the inflammation of the colon, often leading to abdominal pain, diarrhea, and various digestive complications that can disrupt daily routines.
- Common indicators of colon inflammation include diarrhea, abdominal pain, blood in the stool, and weight loss, all of which necessitate immediate medical attention to avert potential complications.
- Colitis triggers can encompass infections, autoimmune responses, and inflammatory bowel diseases such as Crohn's disease and ulcerative colitis.
- Risk factors that may heighten your chance of developing intestinal inflammation include a family history of the disease, some medications, and a personal history of autoimmune disorders.
- Common diagnostic techniques for colitis typically involve blood tests, stool analyses, colonoscopy, and imaging methods such as CT scans and MRIs.
 Recognizing and Addressing the Distressing Symptoms Associated with Colitis
Recognizing and Addressing the Distressing Symptoms Associated with Colitis
The symptoms linked to colitis can be extremely distressing and may vary widely among individuals. A common symptom is abdominal pain, which can fluctuate from mild discomfort to severe cramping. This pain frequently coincides with other gastrointestinal issues, complicating the process of pinpointing the exact cause and leading to heightened frustration and anxiety in affected individuals.
Chronic diarrhea is another prevalent symptom that may occur along with blood or mucus in the stool. Such occurrences can produce feelings of embarrassment and anxiety, hindering social interactions and negatively affecting your overall quality of life. In addition to abdominal pain and diarrhea, you may also encounter other symptoms like fatigue, weight loss, and a significant decrease in appetite.
These symptoms generally arise as a result of the body’s inflammatory response, compounded by nutritional deficiencies resulting from malabsorption. You may also experience an urgent need to have a bowel movement, which can create anxiety about finding restrooms promptly. Early recognition of these symptoms is crucial in seeking immediate medical care, which can significantly improve your condition and enhance your quality of life.
Investigating the Root Causes of Colitis
While the exact causes of colitis remain somewhat elusive, several factors have been identified as potential contributors to its onset. One major factor is infections caused by bacteria, viruses, or parasites, which can incite inflammation within the colon. These infections trigger an immune response that may present as a range of colitis symptoms, often necessitating prompt medical attention.
If you have experienced gastrointestinal issues after consuming contaminated food or water, it is advisable to consult your healthcare provider for a thorough assessment. Another major contributor to colitis is autoimmune disorders, in which the immune system erroneously attacks healthy cells in the colon. In conditions such as ulcerative colitis and Crohn's disease, the immune response can become dysregulated, resulting in chronic and debilitating inflammation.
Genetic factors are also significant; if you have a family history of inflammatory bowel disease, your risk of developing intestinal inflammation may be increased. By understanding these underlying causes, you can collaborate with your healthcare team to create a personalized treatment plan that effectively addresses your specific health needs.
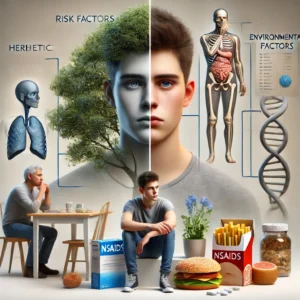 Identifying and Comprehending the Risk Factors Associated with Colitis Development
Identifying and Comprehending the Risk Factors Associated with Colitis Development
Several risk factors can elevate your chances of experiencing colon inflammation. Age is a crucial element; while IBD (Inflammatory Bowel Disease) can develop at any age, it is predominantly diagnosed in individuals between the ages of 15 and 30. Additionally, a family history of inflammatory bowel disease can amplify your risk due to genetic predispositions.
Environmental factors, including dietary habits and lifestyle choices, also play a significant role in the emergence of colitis. Certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), have been linked to a heightened risk of colitis. If you frequently use these medications for pain relief, it may be wise to discuss alternative options with your healthcare provider to mitigate this risk.
Moreover, smoking has been recognized as a risk factor for Crohn's disease, although it may offer a protective effect against ulcerative colitis. By understanding these risk factors, you position yourself to make informed health decisions and implement effective preventative measures.
Innovative Diagnostic Techniques for Accurate Identification of Colitis
Diagnosing colitis typically involves a thorough evaluation that includes a review of your medical history, a physical examination, and various diagnostic tools. One cutting-edge method that has gained traction is Breath Gas Chromatography (BGC), a non-invasive technique that identifies gastrointestinal disorders. This advanced method examines gases in your breath to detect specific biomarkers linked to colonic inflammation, providing a new perspective on diagnostics.
Employing BGC allows healthcare providers to gather important insights into your condition without subjecting you to invasive procedures. Traditional diagnostic methods include colonoscopy and imaging studies such as CT scans or MRIs. During a colonoscopy, a flexible tube equipped with a camera is introduced to inspect the lining of your colon directly.
This approach enables healthcare professionals to visualize any inflammation or lesions present in the colon. Although effective, these methods can be uncomfortable and often require preparation that some individuals may find challenging. The rise of Breath Gas Chromatography marks a promising advancement in early detection and personalized treatment strategies for managing IBD (Inflammatory Bowel Disease).
Custom-Tailored Treatment Approaches for Managing Colon Inflammation
When addressing colon inflammation, a standardized treatment approach is insufficient; treatment plans must be tailored to accommodate your specific requirements and the severity of your condition. Medications are often prescribed to effectively manage inflammation and alleviate symptoms. Anti-inflammatory drugs, especially aminosalicylates, are frequently used as first-line therapies for mild to moderate cases of ulcerative colitis.
For more severe situations or when initial treatments fail to provide relief, corticosteroids or immunosuppressants may be recommended to control symptoms. In certain instances, surgical intervention may be necessary, particularly if complications arise or if medical management does not yield satisfactory results. Surgical options can range from resection of affected areas of the colon to the creation of an ostomy bag for waste elimination.
While surgery can effectively alleviate symptoms, it is typically considered a last resort after other treatment avenues have been explored. Collaborating closely with your healthcare team ensures that you receive the most suitable treatment tailored to your individual circumstances, ultimately improving your health and overall well-being.
 Implementing Strategic Lifestyle Changes to Enhance Colitis Management
Implementing Strategic Lifestyle Changes to Enhance Colitis Management
Beyond medical treatments, adopting specific lifestyle modifications can significantly improve your quality of life while managing the symptoms of bowel inflammation. Diet is a critical factor; many individuals discover that certain foods can worsen their symptoms, while others may provide relief. Keeping a detailed food diary can aid in recognizing potential triggers and guiding you toward informed dietary choices.
Some individuals may find a high-fiber diet beneficial, whereas others might need to limit high-fiber foods, especially during flare-ups. Stress management is another essential component of living with colitis. Since stress can exacerbate symptoms and trigger flare-ups, incorporating relaxation techniques such as yoga, meditation, or deep breathing exercises into your daily routine can be extremely helpful.
Regular physical activity is also vital; moderate exercise can promote digestion and enhance overall well-being. By embracing these lifestyle changes, you can take proactive steps to manage your condition effectively and improve your overall quality of life.
The Grave Consequences of Ignoring Intestinal Inflammation
If bowel inflammation is neglected, it can lead to serious complications that may profoundly affect your health. One significant risk is the potential development of colorectal cancer, especially in individuals with prolonged ulcerative colitis or Crohn's disease that pertains to the colon. Regular screenings are essential for early detection and timely intervention when necessary.
Other complications may include severe dehydration caused by chronic diarrhea or bowel obstructions resulting from inflammation or scarring within the intestines. In rare cases, a condition known as toxic megacolon—characterized by extreme dilation of the colon—can occur. Acknowledging the importance of timely diagnosis and treatment is crucial for preventing these complications and ensuring optimal health outcomes.
Gaining a comprehensive understanding of bowel inflammation—from its symptoms and causes to diagnostic tools and treatment options—empowers you to take control of your health journey. By staying informed and proactive in managing this condition, you can work towards achieving a better quality of life while minimizing the impact of colitis on your daily activities.
Your Questions Answered: Frequently Asked Questions Regarding Colitis
How is colitis defined in medical terms?
Colitis is a medical term that denotes inflammation of the colon, also known as the large intestine. This inflammation can lead to a wide range of symptoms, appearing in both chronic and acute forms that necessitate careful management and effective treatment.
What symptoms should I be vigilant about concerning colitis?
Symptoms related to colitis may encompass abdominal pain, diarrhea, rectal bleeding, weight loss, fatigue, and fever. The intensity and frequency of these symptoms can vary significantly based on the individual and the specific type of colitis they are experiencing.
What are the prevalent causes of colitis?
Colitis can arise from various factors, including autoimmune reactions, infections, and inflammatory bowel diseases such as Crohn's disease and ulcerative colitis. Other potential causes may include ischemic colitis, radiation colitis, and microscopic colitis.
How is colitis accurately diagnosed in a clinical setting?
Colitis is diagnosed through a combination of assessing medical history, conducting a physical examination, performing blood tests, stool tests, and utilizing imaging studies such as CT scans or colonoscopies, along with tissue biopsies. These diagnostic methods are critical for determining the underlying cause and severity of IBD (Inflammatory Bowel Disease).
Presented By: Colitis Diagnosis
The Article: Colitis: Key Symptoms, Causes, and Diagnosis Explained appeared first on https://mcrtherapies.co.uk
The Article Colitis Symptoms, Causes, and Diagnosis Uncovered appeared first on https://mcrtherapies.com
The Article Colitis Symptoms: Causes and Diagnosis Explained Was Found On https://limitsofstrategy.com


Comments are closed